The 2019 Eastern Equine Encephalitis Virus Outbreak in Massachusetts: A Spatial Analysis
Related Articles: The 2019 Eastern Equine Encephalitis Virus Outbreak in Massachusetts: A Spatial Analysis
Introduction
With enthusiasm, let’s navigate through the intriguing topic related to The 2019 Eastern Equine Encephalitis Virus Outbreak in Massachusetts: A Spatial Analysis. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
The 2019 Eastern Equine Encephalitis Virus Outbreak in Massachusetts: A Spatial Analysis

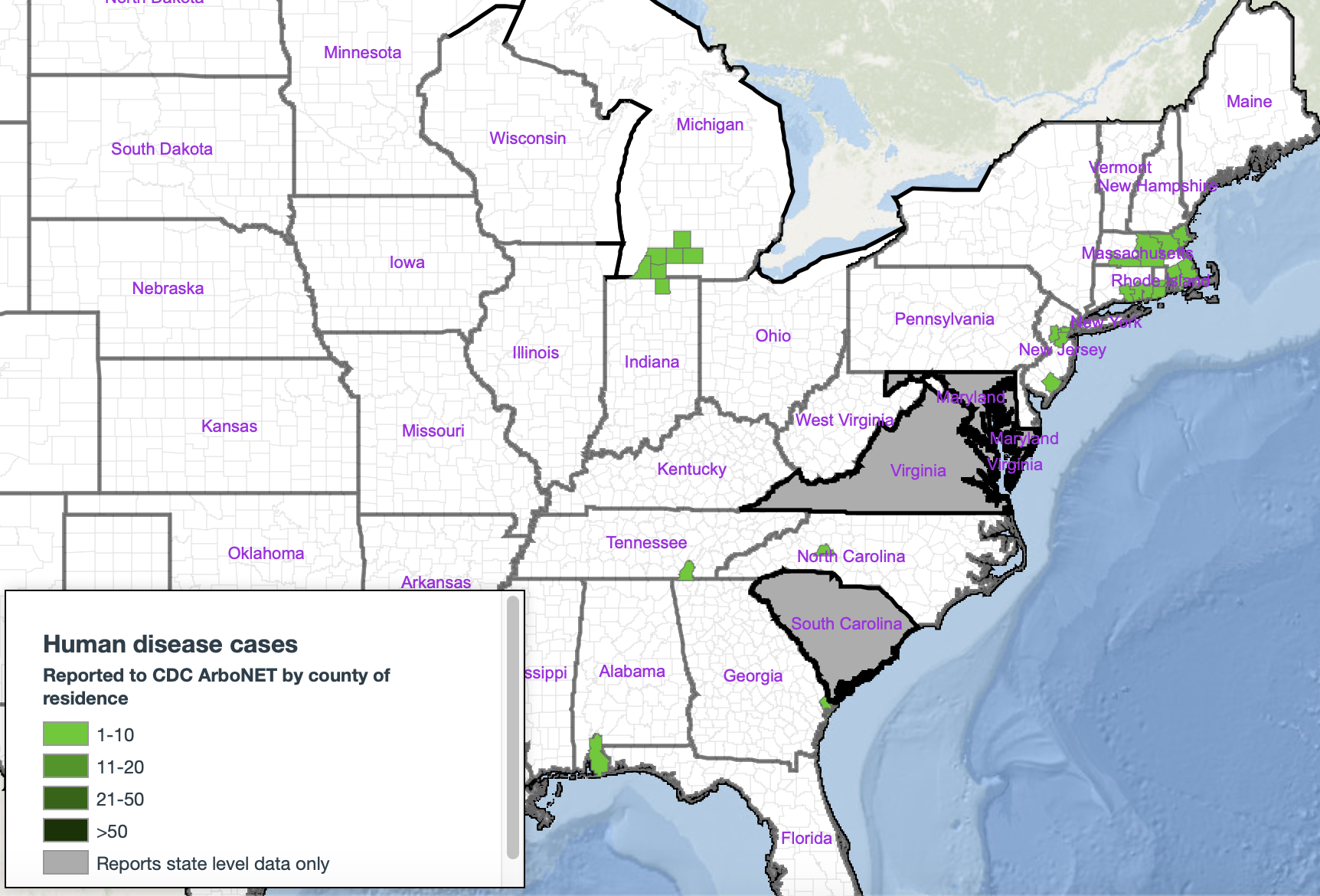
The year 2019 witnessed a significant increase in Eastern Equine Encephalitis (EEE) virus activity in Massachusetts, prompting heightened public health concerns and intensive surveillance efforts. Understanding the spatial distribution of the virus during this period is crucial for effective disease prevention and control strategies. Analysis of the geographical data from that year reveals critical insights into the outbreak’s characteristics and informs future preparedness measures.
Understanding the Data and its Limitations
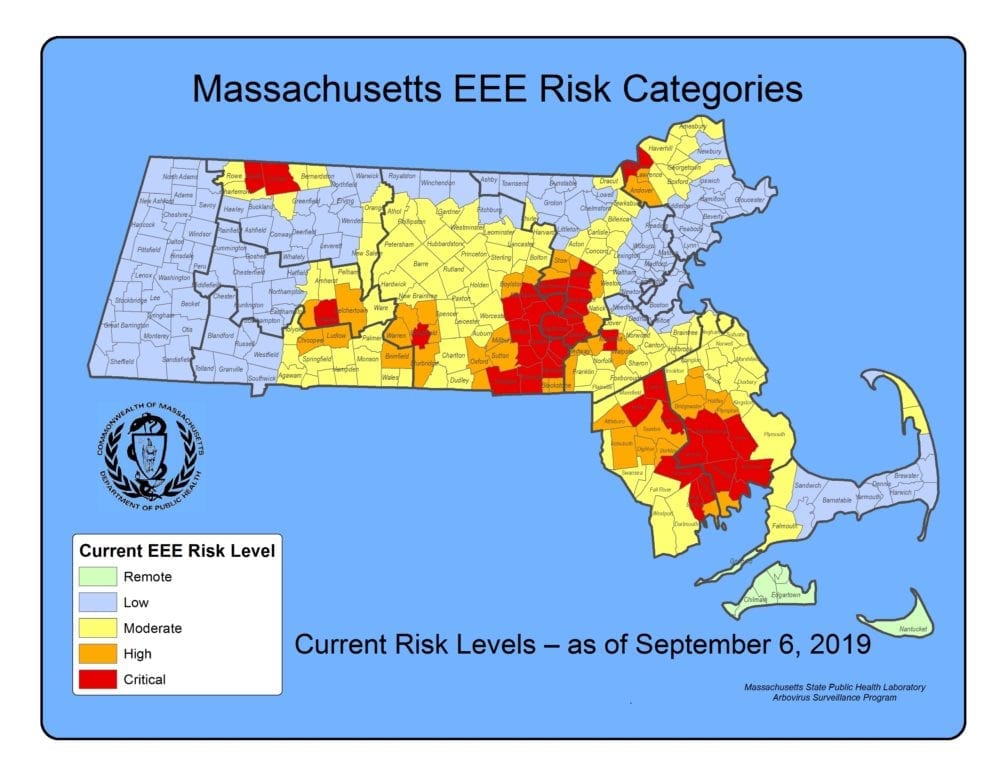
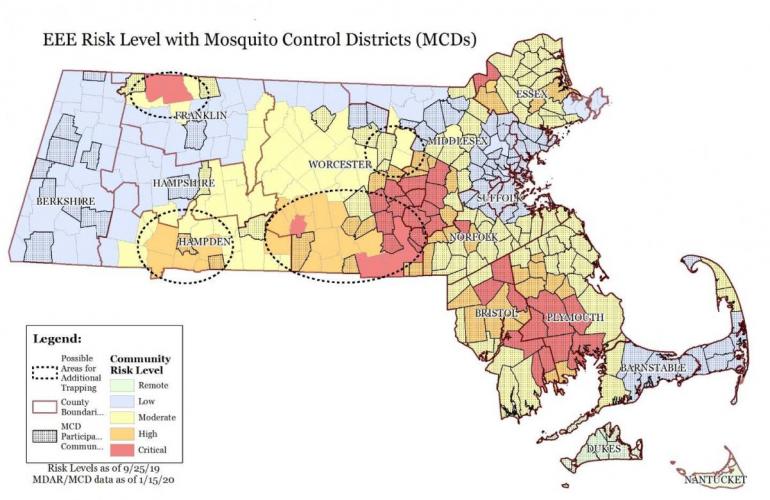
Data on EEE virus activity in 2019, including confirmed human cases, animal infections, and mosquito surveillance results, were collected and analyzed by the Massachusetts Department of Public Health (MDPH) and other collaborating agencies. This information, typically visualized through geographic information systems (GIS), allowed for the creation of maps depicting the spatial distribution of the virus. These maps illustrated areas with higher concentrations of cases and positive mosquito pools, identifying high-risk zones.
However, it is essential to acknowledge the limitations of such data. The observed spatial distribution reflects the extent of surveillance and testing conducted, not necessarily the true extent of viral circulation. Areas with limited surveillance may underestimate the actual number of cases. Furthermore, the identification of infected mosquitoes doesn’t directly translate to human infection risk, as other factors, including environmental conditions and individual exposure levels, play significant roles.
Key Findings from the 2019 Spatial Analysis
The 2019 maps highlighted a cluster of EEE cases and positive mosquito pools in southeastern Massachusetts. This region experienced a disproportionately high number of human infections compared to other parts of the state. This spatial clustering indicated a localized, high-intensity outbreak. Analysis likely revealed specific towns and counties with the highest incidence rates, enabling targeted public health interventions.
The data also illuminated the importance of environmental factors. The spatial distribution of cases and positive mosquito pools likely correlated with wetland areas and other habitats favorable for mosquito breeding. This understanding helped identify areas requiring enhanced mosquito control measures. Analysis may have shown a relationship between specific mosquito species and the observed outbreak, informing targeted vector control strategies.
Public Health Response and its Spatial Implications
The maps generated from the 2019 data guided the public health response in several ways. High-risk areas identified through spatial analysis became the focus of intensified mosquito control efforts, including larviciding and adulticiding programs. Public health officials also used this information to target public awareness campaigns, providing specific guidance to residents in affected areas on how to protect themselves from mosquito bites.
The spatial data also informed decisions regarding the allocation of resources, ensuring that areas with the highest risk received the necessary support for mosquito surveillance, control, and public health education. This targeted approach maximized the efficiency of resource utilization and minimized the impact of the outbreak.
Frequently Asked Questions
-
Q: What specific geographic areas in Massachusetts were most affected by the 2019 EEE outbreak?
-
A: The southeastern region of the state experienced a disproportionately high number of cases and positive mosquito pools. Specific towns and counties identified as high-risk would be detailed in MDPH reports and publications from that year.
-
Q: Did the maps accurately reflect the true extent of the EEE virus spread in 2019?
-
A: The maps reflected the extent of surveillance and testing conducted. Areas with less intensive surveillance may have underestimated the actual number of infections.
-
Q: What types of data were used to create the maps?
-
A: The maps incorporated data on confirmed human cases, animal infections, and mosquito surveillance results, including the location of positive mosquito pools and the species of mosquitoes involved.
-
Q: How did the spatial analysis of the 2019 data inform public health interventions?
-
A: The analysis identified high-risk areas, guiding the allocation of resources for mosquito control and public health education efforts. It allowed for targeted interventions in areas with the highest incidence rates.
Tips for Reducing EEE Virus Risk
-
Mosquito Control: Implement effective mosquito control measures around homes and properties, including eliminating standing water sources and using EPA-registered insect repellents. Community-level mosquito control programs are also crucial.
-
Protective Clothing: Wear long sleeves, long pants, and socks when outdoors, especially during dawn and dusk, when mosquitoes are most active.
-
Insect Repellent: Use EPA-registered insect repellents containing DEET, picaridin, IR3535, oil of lemon eucalyptus (OLE), or para-menthane-diol (PMD) according to label instructions.
-
Awareness and Education: Stay informed about EEE virus activity in the area through local health departments and public health agencies. Participate in community mosquito surveillance and control programs.
-
Prompt Medical Attention: Seek immediate medical attention if experiencing symptoms suggestive of EEE virus infection, such as fever, headache, stiff neck, and confusion.
Conclusion
The 2019 EEE virus outbreak in Massachusetts underscored the importance of robust surveillance, spatial analysis, and targeted public health interventions. The geographic mapping of the outbreak provided critical insights into the spatial distribution of the virus, guiding resource allocation and informing targeted control measures. Continued surveillance, coupled with effective community engagement and proactive mosquito control strategies, remains crucial for mitigating the risk of future outbreaks. Regular review and refinement of surveillance and response protocols are essential to adapt to the evolving dynamics of EEE virus activity in Massachusetts.





Closure
Thus, we hope this article has provided valuable insights into The 2019 Eastern Equine Encephalitis Virus Outbreak in Massachusetts: A Spatial Analysis. We thank you for taking the time to read this article. See you in our next article!